THORACIC OUTLET SYNDROME AND FROZEN SHOULDER
A frequent reason to visit MY SPORTS INJURY CLINIC is shoulder pain, generally, it is a shoulder injury. There are many different types of shoulder injuries such as frozen shoulder and thoracic outlet syndrome, the last one is accompanied with neck pain as well. Others common shoulder injuries are rotator cuff injury and shoulder impingement.
These shoulder injuries are treated at Sport Massage Manchester City Centre with the best trained staff and equipment of Manchester physio.

In this article you can know, How to treat a shoulder injury when you attend Sport Massage Manchester?
- Physiotherapy Manchester sessions.
- Yoga for shoulder injury.
- Mental health services, etc.
The Physio Manchester experts always say “NO HEALTH WITHOUT MENTAL HEALTH”.
A condition that causes neck and shoulder pain is thoracic outlet syndrome (TOS), it occurs when the nerves or blood vessels just below the neck are compressed or tight. Compression can occur between the neck and shoulder muscles.
Treatment includes physical therapy as shoulder injury exercises, pain relievers and in severe cases, surgery.
In accordance with Michael Rubin (2019) its pathogenesis is often unknown, but it sometimes involves compression of the lower trunk of the brachial plexus (and perhaps the subclavian vessels) but this condition is unclear. Compression can be caused by:
- A cervical rib.
- Abnormal first thoracic vertebra.
- Abnormal position or insertion of the scalene muscles.
- Poorly consolidated clavicle fracture.
Signs and symptoms
There are several types of thoracic outlet syndrome, including the following:
- Neurogenic (neurological) thoracic outlet syndrome. This most common type of thoracic outlet syndrome is brought about by compression of the brachial plexus.
- Vascular thoracic outlet syndrome. This type of thoracic outlet syndrome occurs when one or more of the veins (thoracic venous outlet syndrome) or arteries (thoracic arterial outlet syndrome) below the clavicle become compressed.
- Nonspecific thoracic outlet syndrome. This kind of injury is also called disputed thoracic outlet syndrome. Some doctors do not believe it exists, while others say it is a common disorder.
Symptoms of thoracic outlet syndrome can vary depending on which structures are compressed. When the nerves are compressed, the signs and symptoms of neurological thoracic outlet syndrome include:
- Numbness or tingling in the arm or fingers.
- Pain or discomfort in the neck, shoulder, or hand.
- Weakening of grip.
Signs and symptoms of vascular thoracic outlet syndrome may include:
- Discoloration of the hand (bluish color).
- Swelling and arm pain, possibly due to blood clots.
- Weak pulse in the affected arm.
- Cold fingers, hands or arms.
- Arm fatigue with activity.
Causes of (TOS)
The causes of compression vary and can include the following:
- Anatomical defects.
- Bad posture.
- Trauma injury.
- Repetitive activity, doing the same thing repeatedly can, over time, wear down body tissue.
- Pressure exerted on the joints, obesity can put too much pressure on your joints.
- Pregnancy, because joints loosen during pregnancy, the signs of thoracic outlet syndrome may first appear while you are pregnant.
Diagnosis of thoracic outlet syndrome (TOS)
Diagnosing thoracic outlet syndrome can be difficult because symptoms and their intensity can vary greatly between people who have this disorder.
- Imaging studies and nerve studies, X-rays, ultrasound, CT scan, magnetic resonance imaging (MRI), angiography, arteriography and venography, electromyography, nerve conduction study.
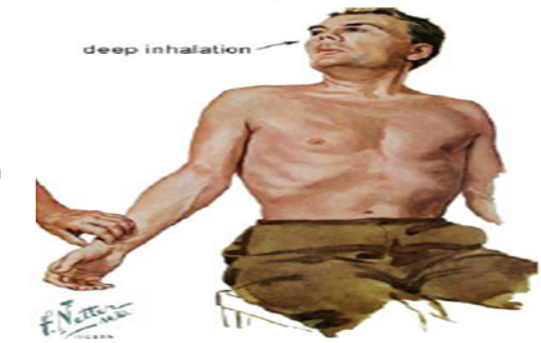
To diagnose thoracic outlet syndrome, your doctor or physical therapist can review your symptoms and medical history and perform a physical exam.
- Physical exploration, a physical examination will be done to look for external signs of thoracic outlet syndrome, such as slumped shoulders, swelling or paleness in the arm, abnormal pulses, or reduced range of motion.
Among the most characteristic tests for (TOS) pathology are those who put in compromise the different gorges through which neurovascular bundle runs.
Treatment of (TOS)
How to heal a shoulder injury like Thoracic Outlet syndrome, in most cases, a conservative treatment modality is effective if your condition is diagnosed early. Shoulder injury treatment may include:
- Physiotherapy, if you have neurogenic thoracic outlet syndrome, physical therapy at sports massage Manchester city Centre may be the treatment of choice.

You will learn with your physio Manchester how to perform exercises to strengthen and stretch the shoulder muscles, thereby, opening the thoracic outlet and improving range of motion and body posture. These exercises, over time, can relieve pressure on the blood vessels and nerves at the (TOS).
- Medication, your doctor may prescribe anti-inflammatory drugs, pain relievers, or muscle relaxants to decrease inflammation and promote muscle relaxation.
If you are diagnosed with thoracic outlet syndrome, your doctor or physical therapist will instruct you to do exercises at home such as yoga for shoulder injury to strengthen and support the muscles around the thoracic outlet and also help to have a good mental health and an acceptable mental health statistics, to finally get a full shoulder injury recovery.

In general, to avoid unnecessary stress on your shoulders and the muscles around the thoracic outlet, you should do the following:
- Maintain good posture.
- Take often breaks at work to move and stretch.
- Avoid mental health crisis.
Wait, surely you must be thinking, what is mental health?
Mental health includes the emotional, psychological and social well-being of people. It affects the way we think, feel, and interact. Understanding this, mental health in UK is an extremely important point; we must keep in mind mental health and become aware of.
- Keep a healthy weight.
- Avoid carrying heavy bags over your shoulder.
- Avoid activities that make symptoms worse or find ways to adapt activities so they don't cause symptoms.
- Create a work area that allows you to maintain good posture and does not make symptoms worse.
- Gently massage the shoulders and thoracic outlet.
- Apply a heating pad to the area.
- Practice relaxation exercises, such as deep breathing, meditation, yoga for shoulder injury and stretching.
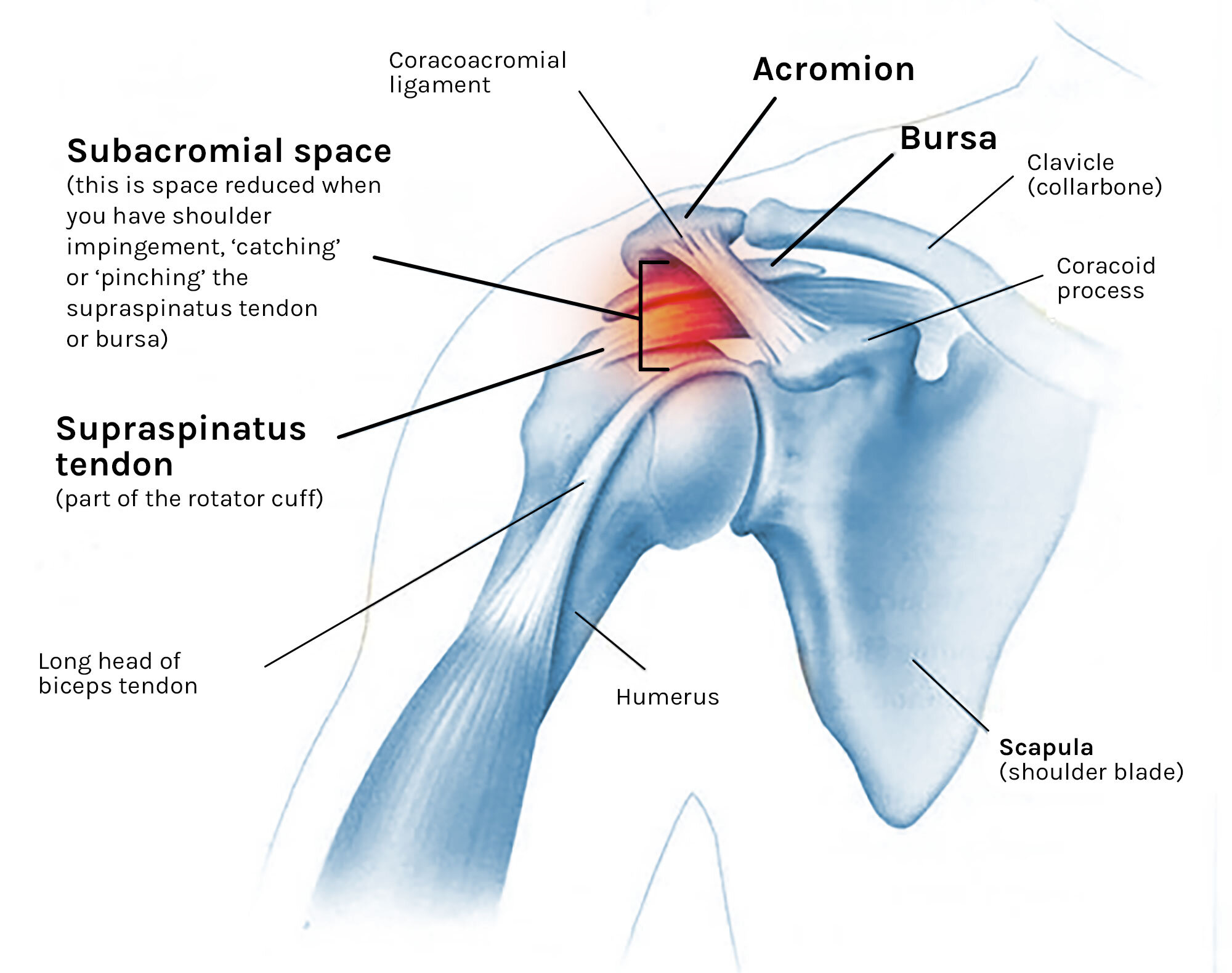
As a result of shoulder pain and loss of motion due to inflammation, we are talking about a condition that it is called frozen shoulder.
In order to Pietro Tonino (2016) people who have frozen shoulder often experience shoulder pain, stiffness, and decreased range of motion. Everyday activities such as getting dressed or reaching for something can be challenging.
The shoulder joint is a ball and socket joint, made up of three bones: the humerus, the shoulder blade, and the clavicle.
Signs and symptoms
- Pain; a dull, fixed and continuous pain that occurs more at night and causes decreased arm movements. More is produced in the first stage.
- Stiffness; greatly limiting arm movements such as fastening the bra or combing hair.
- Decreased mobility of the arm; there is decrease in both active and passive arm mobility.
Causes of frozen shoulder
The capsule of the shoulder joint has ligaments that attach the shoulder bones to each other. When capsule inflammation occurs, these bones are unable to move freely in the joint. Most of the time, there is no cause for the inflammation. Risk factors include:

- Diabetes.
- Thyroid problems.
- Changes in your hormones, such as those what happen during menopause.
- Shoulder injury.
- Mental health problems.
- Shoulder surgery.
- Open heart surgery.
- Cervical disc disease of the neck.
Diagnosis of Frozen shoulder
It is usually done with a good medical history and physical examination.
On physical examination, the patient is asked to raise the arms with the palms of the hands up, arms forward (wanting to push something forward), spread the arms to the sides, and bring the hands behind the back. If any of these movements present difficulty, you should think of frozen shoulder. Sometimes doctors and physio Manchester ask for additional studies such as an X-ray or an MRI, this serves to rule out other types of injuries.
Treatment of frozen shoulder
The main treatment is non-steroidal anti-inflammatory drugs, steroid injections, and physical therapy.

When the treatment is not effective, surgery is performed. Physiotherapeutic treatment should always be carried out after surgery; recovery varies from 6 weeks to 3 months.
Physiotherapy Manchester
- Heat; the heat applied at the beginning of the treatment helps to loosen the shoulder before mobilizations and stretches.
- Shoulder mobilizations; your physio Manchester must perform gentle mobilizations.
- Stretching.
- Gentle massages of all the muscles.
- Acupuncture.
- Cryotherapy at the end of the therapies.
Physio exercises for the frozen shoulder patient.
- “Spiderlings”, facing a wall with your hands extended on it, climb with your fingers up as if it were a spider, go up until you feel tension in your shoulder, lower and rest your arm, do this 10 times.
- Codman exercises; recommended at the beginning of therapy and at the end of it. Perform circles with the arm hanging on the table.
- With a stick lying down and seated, perform the movements of flexion, rotation, abduction and adduction of the arm, helping you with the good arm.
- In the frame of a door, place the arm at 90º of flexion and put the hand on the edge of the door, turn the body to cause external rotation at the shoulder.
- Self-assisted arm lift. Positioned supine on the table, bring the arm up and from below the elbow; help with the hand of the good arm to force the movement.
- Cross the outstretched affected arm to the other side passing under the chin and increase the stretch with the hand of the good arm. This can be done on the back with the help of a towel grasped by the ends with both hands and pulling to the right or left to search for internal or external rotation.
References
American Academy of Orthopaedic Surgeons website. Frozen shoulder. Orthoinfo.aaos.org/en/diseases—conditions/frozen-shoulder. Update March 2018. Accessed December 10, 2018.
Finnoff JT. Upper limb pain and dysfunction. In: Cifu DX, ed. Braddom’s Physical Medicine and Rehabilitation. 5th ed. Philadelphia, PA: Elseveir; 2016: chap 35.
Harris JD, Griesser MJ, Jones GL. Stiff shoulder. In: Miller MD, Thompson SR, eds. Delee and Drez’s Orthopaedic Sports Medicine: Principles and Practice. 4th ed. Philadelphia, PA: Elsevier Saunders; 2015: chap 55.
Miller RH, Azar FM, Throckmorton TW. Shoulder and elbow injuries. In: Azar FM, Beaty JH, Canale ST, eds. Campbell’s Operative Orthopaedics, 13th ed. Philadelphia, PA: Elsevier; 2017: chap 46.
Ferri FF. Thoracic outlet syndrome. In: Ferri's Clinical Advisor 2020. Philadelphia, Pa.: Elsevier; 2020. https://www.clinicalkey.com. Accessed July 19, 2019.
Frozen Shoulder. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00071. Last reviewed January 2011. Accessed May 19, 2016.
Manske RC, Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1(3-4):180-9.
Adhesions in the Shoulder. PubMed Health website. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0025850/. Accessed May 22, 2016.
Page P, Labbe A. Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther. 2010;5(4):266-73.
Andary J.L, Petersen S.A.The vascular anatomy of the glenohumeral capsule and ligaments: an anatomic study. J Bone Joint Surg Am. 2002; 84-A: 2258-2265.
Buller LT, et al. Thoracic outlet syndrome: Current concepts, imaging features, and therapeutic strategies. The American Journal of Orthopedics. 2015;44:376.
AskMayoExpert. Thoracic outlet syndrome. Rochester, Minn.: Mayo Foundation for Medical Education and Research; 2019.
Grunebach H, et al. Thoracic outlet syndrome. Vascular Medicine. 2015;20:493.