HOW MY SPORTS INJURY PHYSIOTHERAPIST ADDRESS NEUROMUSCULAR DEFICIT GAIT DISORDERS: WHAT YOU SHOULD KNOW
To most of us, walking feels like the most natural, carefree movement. But there is a lot of work that goes into each careful step, through our strength, coordination, and balance. Walking is an extraordinarily complex task requiring integration of the entire nervous system, making gait susceptible to a variety of underlying neurologic abnormalities (Baker 2018). They depend on different parts of the body's proper operation. Eyes, hearing, the brain, and muscles are a few of these. These troublesome areas can result in difficulties walking, falls, or injuries if not handled or thoroughly assessed. Expert physiotherapists claim that determining the underlying reasons of gait abnormalities requires more time. My sports injury's physiotherapists place a strong emphasis on gait analysis and its primary therapeutic role, thereby bulletproof your walking gait movement for anything life throws at you.

Causes Of Gait and Balance Problems
A combination of a deficiency and attempts at compensating leads to specific characteristics of aberrant gaits.
Muscular neurological problems frequently have long-term consequences.
Problems with gait, balance, and coordination are often caused by specific conditions, which include:
· Parkinson’s disease
· Guillain Barre
· Cerebral Palsy
· Multiple Sclerosis
· Brain haemorrhage
· Brain tumor
· Joint pain or conditions, such as arthritis
· Myopathy
· Spinal cord compression or infraction
· Vit B12 deficiency
· Obesity
· Chronic alcohol abuse
· Usage of hypertensives
Gait and balance problems can be a result of pain, muscles weakness, muscle tightness or spasticity, poor posture, or loss of balance. Muscle weakness can occur in one leg or both and make walking difficult. My Sports Injury's physiotherapists perform techniques to assist your muscles and joints function to their best capacity, enhancing flexibility and muscle strength while reducing pain and stiffness. They use manual hands on tehcniques like soft tissue massage, acupuncture, deep tissue massage, mobilisation, and trigger point release. They also plan rehabilitation exercises to build muscle strength and lower the risk of falling, as well as stretching exercises to lengthen tense muscles and lessen muscle spasms. Moreover, stretching will increase joint flexibility and your capacity for walking. To help you reach your full potential, a comprehensive treatment plan involving rehabilitation objectives will be created.
There is experimental evidence that different types of human motor behaviour are organised based on the flexible activation of muscle groups called modules (Giszter et al. 2010; Lacquaniti et al. 2012). It was found both invariant and variant features related to the need to compensate for body weight, provide forward and lateral stability, and maintain forward progression (Ivanenko et al. 2013).
Waddling Gait Biomechanics
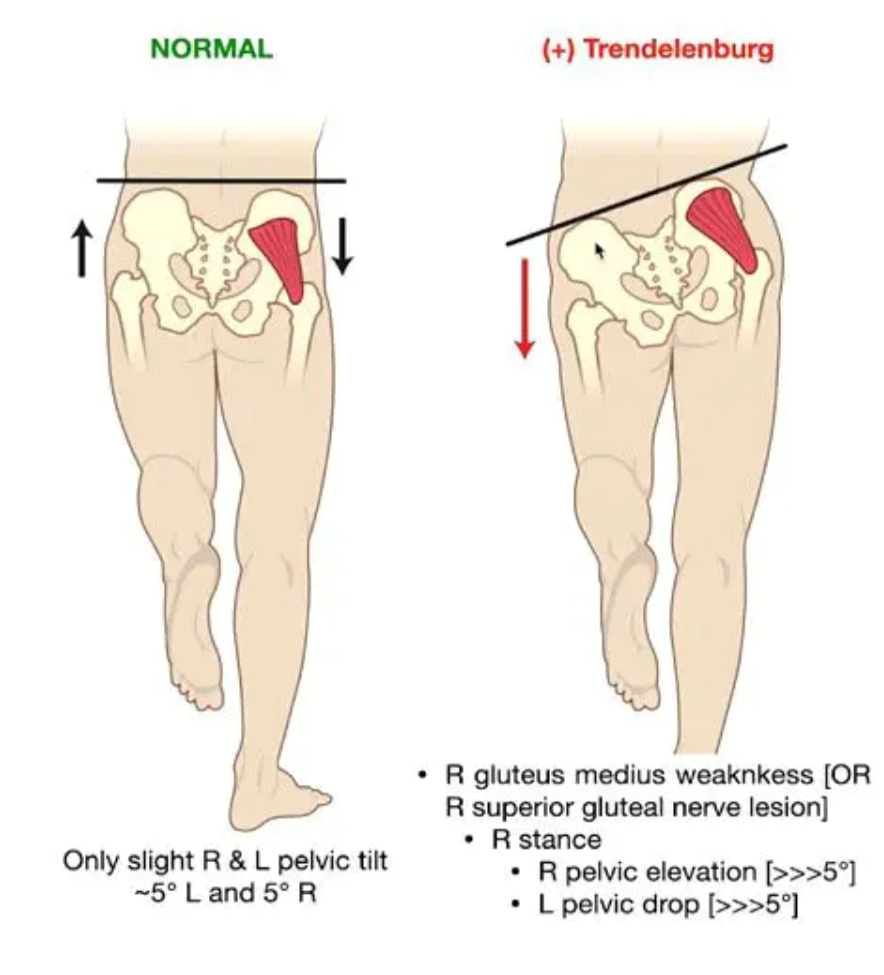
TRENDELENBURG SIGN - Drop of Pelvis when lifting leg opposite to weak gluteus Medius.
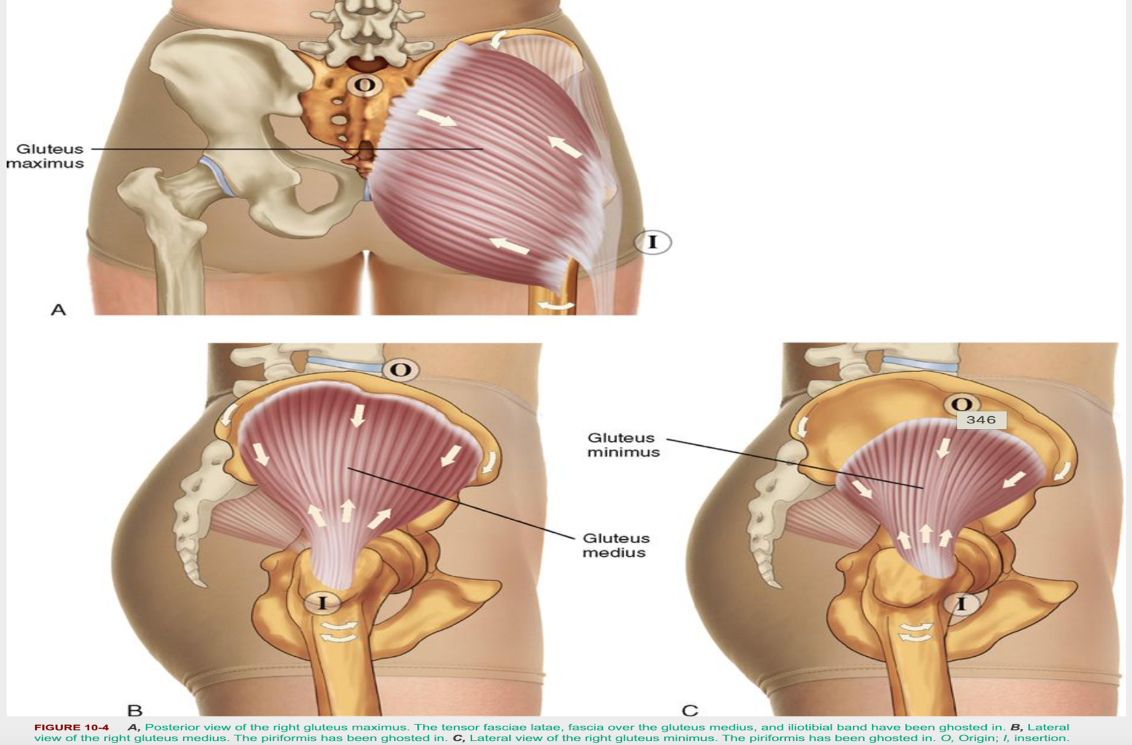
This illustrates the weakened/poor motor of the muscles (HIP ABDUCTORS) involved
2 movement strategies exhibited, both of which are:
1. The first strategy (Trendelenburg)is a manifestation of a pelvic drop, in which the pelvis on the same side as the limb that is swinging forward (swing phase) will DROP. This is because the recruitment of the hip abductors of the stance limb (the leg in contact with the ground) is less than optimal to maintain a level pelvis. This leads to excessive side-to-side trunk motion, giving the gait a waddling appearance.
2. The second strategy (Compensated Trendelenburg) is a manifestation of a trunk lean towards the stance limb. This movement strategy brings my centre of mass over my base of support (the stance foot). This is a compensatory strategy to decrease the external moment (demand) that gravity will put on my hip abductors aka making it easier for the hip abductors on that side to support the pelvis. Watch this: https://youtu.be/cbPzkqo9H-c
Evidence says as it is difficult to recruit gluteal muscles because of its poor representational area. There is a plethora of ways to strengthen the hip muscles, and there are always ways to make obtainable progressions. It is important to know what level of exercise you should start with, and to progress appropriately from there. You only need average glute- med strength to prevent a Trendelenburg gait pattern yet so many people present with this movement pattern. Hence, it is not so much strengthening, but motor control training is important to prevent this compensatory movement pattern. Therefore, dynamic exercise is a great way to improve with not only strength but also motor control of the hip abductor where the Physios at MY Sports Injury focuses on.
Chiropractic treatment can facilitate the improvement of gait patterns. Physiotherapists deal with complex gait issues in more detail within your assessment & examination. In the context of an athlete more times than not, has more than adequate strength yet they fail to utilise and demonstrate the neuromuscular control necessary to engage the hip abductors during tasks. To see if this is the case, we give the athlete visual, verbal, or manual cues to facilitate hip abductor activation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8572672/
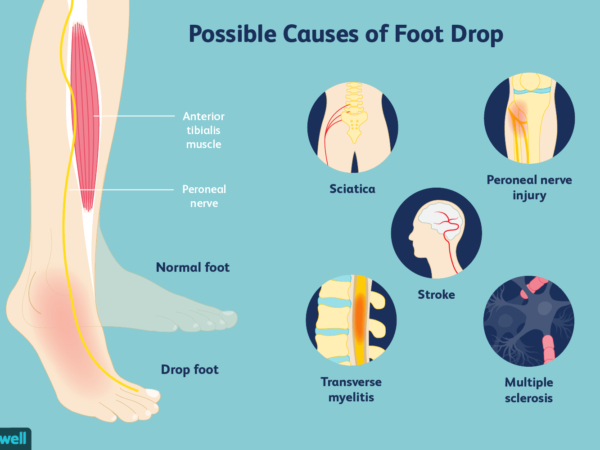
Steppage Gait
The steppage gait is caused by weakness of ankle dorsi-flexors(anterior compartment musculature), also known as a foot drop. Common causes include an L5 radiculopathy or peroneal neuropathy, which can be differentiated from the former by preservation of ankle inversion on physical examination. Because of its superficial location, the peroneal nerve is vulnerable to compression during surgical procedures, tight cast placements, and other traumatic conditions sustained during sports. Patients with diabetes seem to be affected more often.
Watch this: https://youtu.be/R8LRCiTvUz8
Before treatment can be administered for drop foot, physiotherapists at My Sports Injury perform a comprehensive physical examination, review the patient’s medical history, administer neurological evaluations. Treatment depends on the cause and severity of the condition, but generally speaking, pain management may be the first line of treatment. They focuses on strengthening dorsi-flexors, calf muscles, ensures ankle ROM is well maintained. Neuromuscular electrical stimulation help in contracting muscle to have a movement and function properly, stretching of the contracted muscle, MFR, back strengthening exercises, if there is weakness of the anterior tibialis caused by sciatica compression
Assessment of the gait

The physios at My Sports Injury assess gait as when patient as he or she walks from the waiting area to an examination room. Different gait patterns - we might ask the individual to walk normally, on insides and outsides of feet, in a straight line, running (all the time looking to compare sides and understanding of "normal").The gait examination provides significant insight into an individual’s functional status. Also, ask/observe the type of footwear the patient uses(Cranage et al., 2019).
Common Gait Rehab Protocol

Your physiotherapist will focus on re-educating your muscles and joints to weight bear, weight shift and control the leg movement. This will also be done to prevent unwanted compensatory movement. It will also improve your functional ability by facilitating the way you walk. This involves:
· Exercises to help regain standing balance and proprioception
· Muscle strength training Primarily target the muscles that are responsible for gait, weakness of muscles can lead to variety of abnormality. Progressive resisted exercise using weight cuff, theraband, resistance tube
· Stretching to increase range of movement
· Walking through doorways, and on different surfaces
· Auditory and Visual stimuli to encourage you to take bigger steps and reduce the effects of freezing. For example, mirror imaging or modulating gait with a metronome (a device that produces regular beats) (Baram. 2013)
· Activities to increase the magnitude of the step and the amplitude of the movement (Noh et al,. 2018)
· Breaking the gait cycle down into smaller more manageable chunks and repeating movement to stimulate nerve pathways
· Obstacle gait Training
· Target stepping
· Visual feedback- (Koldenhaven et al., 2020)
· Kinesio taping on trunk (Lee et al,. 2016)
My Sports Injury & physiotherapy is a private physical health clinic in the heart of Manchester, we are committed to promote efficient pain control, higher functioning of body movement, and better quality of life! If you’re suffering from gait abnormalities don't hesitate to contact us to give you support & guidance; our qualified specialist physiotherapy team can give you exact evidence-based treatment and pain-management required.
You may visit www.mysportsinjury.co.uk to make a booking Now – FREE Customer Consultation in your initial Appointment.
References:
· Bowley MP, Doughty CT. Entrapment Neuropathies of the Lower Extremity. Med Clin North Am. 2019 Mar;103(2):371-382
· Giszter SF, Hart CB, Silfies SP. Spinal cord modularity: evolution, development, and optimization and the possible relevance to low back pain in man. Exp Brain Res 200: 283–306, 2010.
· Ivanenko YP, Cappellini G, Solopova IA, Grishin AA, MacLellan MJ, Poppele RE, Lacquaniti F. Plasticity and modular control of locomotor patterns in neurological disorders with motor deficits. Front Comput Neurosci 7: 123, 201
· Jessica M. Baker, Gait Disorders, The American Journal of Medicine, Volume 131, Issue 6, 2018, Pages 602-607, ISSN 0002-9343, https://doi.org/10.1016/j.amjmed.2017.11.051
· Lacquaniti F, Ivanenko YP, Zago M. Patterned control of human locomotion. J Physiol 590: 2189 –2199, 2012.
· Martino G, Ivanenko YP, Serrao M, Ranavolo A, d’Avella A, Draicchio F, Conte C, Casali C, Lacquaniti F. Locomotor patterns in cerebellar ataxia. J Neurophysiology 112: 2810 –2821, 2014.
· Nath RK, Somasundaram C. Gait Improvements After Peroneal or Tibial Nerve Transfer in Patients with Foot Drop: A Retrospective Study. Eplasty. 2017;17:e31





