Why Weak Hips Are the Hidden Cause of Your Knee Pain (and How to Fix It)
Why Weak Hips Are the Hidden Cause of Your Knee Pain by Aishwarya Antony, MSc Physiotherapy, HCPC Registered Physiotherapist, Manchester
Introduction
Knee pain is one of the most common musculoskeletal complaints seen in both athletes and the general population. While many people focus directly on the knee joint when pain develops, the true source of the problem often lies higher up the kinetic chain in the hips.
The hip plays a crucial role in maintaining proper lower limb alignment and stability during walking, running, and other activities. Weakness or poor control of the hip muscles can lead to faulty knee mechanics, increasing stress on the structures around the knee and causing pain over time.
forms a key part of physiotherapy rehabilitation Understanding the link between the hips and knees helps explain why targeted hip strengthening for many knee conditions.
The Biomechanical Connection Between the Hips and Knees
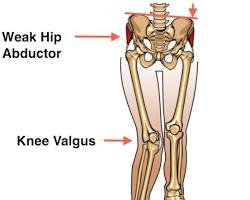
The hip joint provides the foundation for lower limb movement. The main stabilisers particularly the gluteus medius, gluteus maximus, and deep external rotators control the position of the femur during motion.
When these muscles are weak or delayed in activation, the thigh tends to rotate inward and the knee collapses toward the midline, a movement known as dynamic knee valgus [1,2]. This abnormal alignment increases load on the patellofemoral joint, irritates soft tissues around the knee, and can lead to pain syndromes such as patellofemoral pain syndrome (PFPS) or iliotibial band syndrome (ITBS) [3].
In sports, poor hip control can also raise the risk of ligament injuries such as ACL tears, particularly in athletes performing cutting or jumping movements [4].
Essentially, the knee follows where the hip leads and if the hip is unstable, the knee pays the price.
Common Signs of Hip Weakness Contributing to Knee Pain
Patients with hip-related knee issues often show specific patterns during movement, such as:
- Knees moving inward during squats, lunges, or step-downs
- Poor balance or control on one leg
- Pain around or behind the kneecap, especially during stairs or prolonged sitting
- Hip or groin tightness alongside knee discomfort
These movement patterns indicate that the hip muscles are not adequately supporting the knee joint during dynamic activities.
How Physiotherapy Helps: A Holistic Approach
Physiotherapy treatment for knee pain linked to hip weakness aims to restore muscle balance, stability, and movement control throughout the lower limb. The process generally involves several phases.
1. Assessment and Movement Analysis
A physiotherapist begins by identifying faulty movement patterns through gait analysis, single-leg balance tests, and functional movements like squats or step-downs.
Specific muscle testing can determine whether the gluteal or deep hip stabilisers are underactive or weak. This assessment guides the design of an individualised rehabilitation programme [5].
2. Activation and Motor Control Training
Before strengthening, the goal is to “reconnect” the brain and hip muscles. This involves low-load, controlled exercises to improve activation of the glutes and deep rotators. Examples include:
- Glute bridges (with focus on symmetrical activation)
- Clamshells and side-lying hip abduction
- Hip external rotation with resistance bands
These movements help retrain the neuromuscular system and prepare the body for more advanced exercises.
3. Progressive Strengthening
Once activation is established, progressive strengthening builds endurance and control. Key exercises include:
- Lateral band walks and monster walks for the gluteus medius
- Single-leg squats and step-ups for dynamic stability
- Hip thrusts and deadlifts for gluteus maximus strength
Research shows that combining hip and knee strengthening is more effective for reducing anterior knee pain than focusing on the knee alone [6,7].
Physiotherapists often emphasise proper technique ensuring knees track over toes and avoiding inward collapse — to promote correct movement patterns.
4. Movement Retraining and Functional Integration
After strength improves, retraining full-body coordination is essential. Patients practise movement control during running, jumping, and sport-specific drills.
Video feedback or mirror training may be used to enhance body awareness and correct faulty alignment. The goal is to make new movement patterns automatic, preventing the recurrence of pain and injury [8].
5. Prevention and Maintenance
Once symptoms settle, maintaining hip strength remains vital. Integrating gluteal exercises into regular workouts and staying aware of posture during daily tasks such as standing, walking, or climbing stairs helps preserve joint health.
Simple strategies like warming up before activity, avoiding prolonged sitting, and cross-training can further reduce strain on the knees.
Who Benefits the Most from Hip Strengthening?
Hip-focused rehabilitation is effective for a wide range of individuals:
- Runners and athletes experiencing patellofemoral pain or IT band syndrome
- Gym-goers with knee discomfort during squats or lunges
- Office workers with weak glutes due to prolonged sitting
- Post-surgical patients recovering from ACL or knee arthroscopy
By addressing the root cause rather than just the symptoms, physiotherapy provides long-term improvement in function and performance.
The Bigger Picture: Why the Hip Matters for Whole-Body Health
The hip is a powerful driver of movement efficiency. When it functions well, it distributes forces evenly through the kinetic chain, protecting not just the knee but also the lower back and ankles.
Neglecting hip strength, on the other hand, can lead to a cascade of compensations altered gait, overuse of smaller muscles, and joint overload. Strengthening the hips supports optimal biomechanics, enhances stability, and improves overall mobility and posture [9].
Conclusion
Strong hips form the foundation for healthy knees. By improving hip strength and control, you reduce abnormal stress on the knee joint, enhance performance, and prevent injuries.
Physiotherapy plays a crucial role in identifying weaknesses, guiding proper exercise progression, and ensuring safe, long-term results.
Whether you’re an athlete or someone dealing with everyday knee pain, focusing on the hips can make all the difference. As physiotherapists often say — happy hips, happy knees!
Book in with HCPC registered Physiotherapist Aishwariya
References
- Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42–51.
- Hollman JH et al. Relationships between knee valgus, hip-muscle strength, and hip-muscle activation during single-leg tasks. J Sport Rehabil. 2009;18(1):104–20.
- Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and on pain in females with patellofemoral pain. J Orthop Sports Phys Ther. 2011;41(9):625–32.
- Hewett TE et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict ACL injury risk. Am J Sports Med. 2005;33(4):492–501.
- Reiman MP, Bolgla LA, Loudon JK. A literature review of studies evaluating gluteus maximus and medius activation during rehabilitation exercises. Phys Ther Sport. 2012;13(3):196–203.
- Dolak KL et al. Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with PFPS. J Orthop Sports Phys Ther. 2011;41(8):560–70.
- Ferber R, Bolgla L, Earl-Boehm J, Emery C, Hamstra-Wright K. Strengthening of the hip and knee musculature in persons with patellofemoral pain. J Athl Train. 2015;50(4):377–91.
- Baldon R de M et al. Effects of functional stabilization training on lower limb biomechanics in women. Med Sci Sports Exerc. 2012;44(1):135–45.
- Semciw AI, Green RA, Murley GS, Pizzari T. Gluteus medius and minimus exercise rehabilitation strategies: a systematic review. Br J Sports Med. 2016;50(10):621–30.
