Hoffa’s Fat Pad Syndrome: Causes, Symptoms, and Physiotherapy Knee Treatment
Hoffa’s Fat Pad Syndrome: Causes, Symptoms, and Physiotherapy Treatment for the Knee by BPT Aishwarya Antony Physiotherapist Manchester (HCPC) MSc BPT
Learn how physiotherapy treats Hoffa’s fat pad syndrome. Discover causes, symptoms, and effective rehab strategies to relieve anterior knee pain and restore function.
Introduction
The knee is a complex joint, and sometimes, even small structures within it can cause big problems. One such structure is Hoffa’s fat pad, a small cushion of fatty tissue located just below the kneecap. When irritated or inflamed, it leads to a condition known as Hoffa’s fat pad syndrome, which can cause persistent anterior knee pain.
Whether you’re an active individual or a desk-bound office worker, understanding this condition and how physiotherapy can help is vital for recovery and preventing future issues.
What Is Hoffa’s Fat Pad and Why Does It Matter?
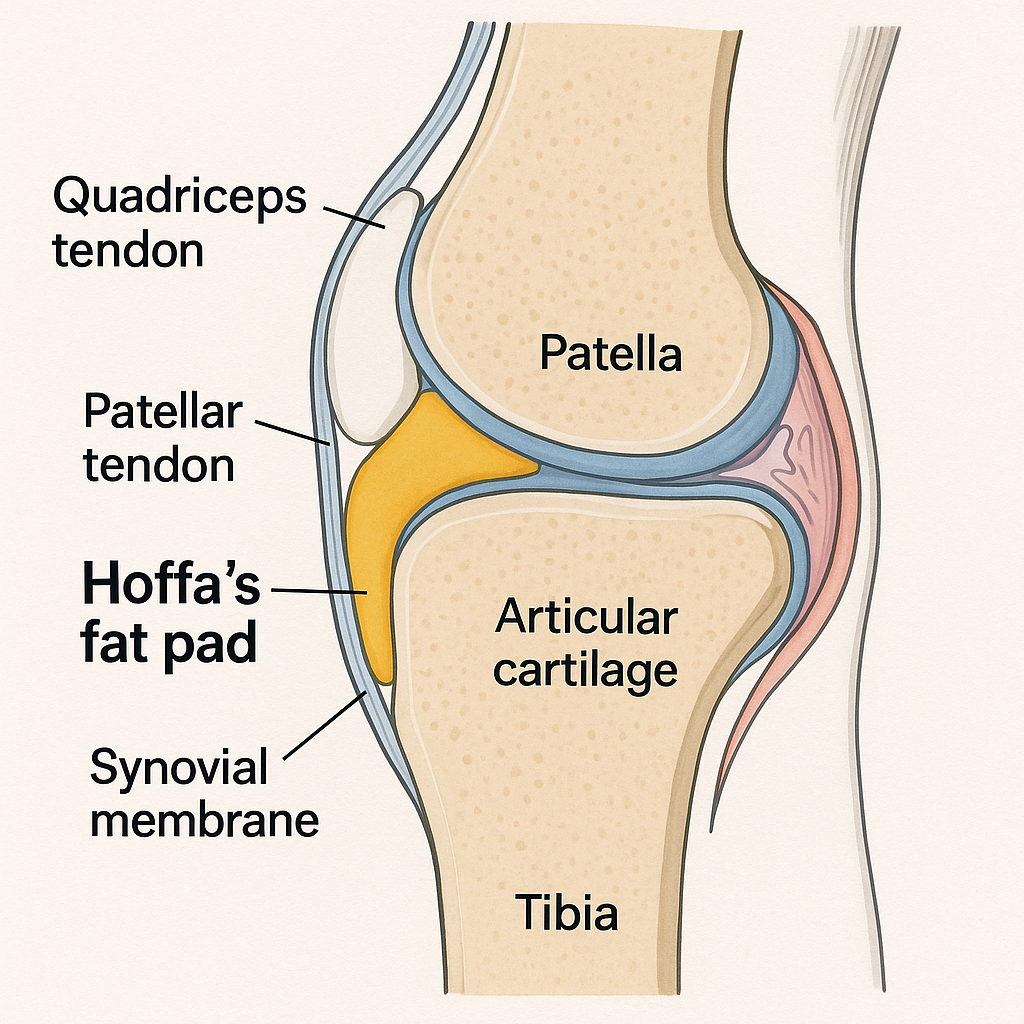
Hoffa’s fat pad, or the infrapatellar fat pad (IFP), sits inside the knee joint capsule but outside the synovial lining. It’s bordered by the patella above, the patellar tendon in front, and the femoral condyles behind [1,2]. Acting like a natural shock absorber, it cushions the knee during movements such as bending and straightening.
When functioning well, it glides smoothly and causes no discomfort. However, when irritated through injury, repetitive stress, or poor knee mechanics, the fat pad can swell and become painful. This inflammation is what we call Hoffa’s fat pad syndrome [3].
Causes and Risk Factors of Hoffa’s Fat Pad Syndrome
The syndrome typically arises from a mix of factors, including:
- Repetitive microtrauma: Activities like running, jumping, or kneeling can cause repeated irritation.
- Mechanical impingement: Poor tracking of the kneecap (patella) can compress the fat pad between bone and tendon.
- Post-surgical changes: Scarring or swelling after knee surgery may involve the fat pad.
- Biomechanical imbalances: Weak hip or thigh muscles and poor lower limb alignment increase stress on the fat pad [4,5].
Sedentary workers may also develop issues due to prolonged sitting, leading to tight muscles and poor knee posture, making the joint more vulnerable during movement.
Signs and Symptoms to Watch For
Common symptoms include:
- Anterior knee pain just below the kneecap, worsening during bending activities like squatting, stair climbing, or prolonged standing.
- Tenderness and swelling around the front of the knee.
- A feeling of tightness or stiffness, especially after rest.
- Reduced range of motion in some cases.
If left untreated, these symptoms may worsen and interfere with daily activities and exercise. MRI scans often reveal swelling or increased signal in the fat pad, confirming inflammation [9].
How Physiotherapy Helps: A Targeted Approach
Physiotherapy offers an effective, non-surgical way to manage Hoffa’s fat pad syndrome. The approach is multi-faceted, focusing on reducing pain and inflammation, restoring normal movement, strengthening key muscles, and preventing future injury.

1. Pain and Inflammation Management
In the initial phase, controlling pain and swelling is crucial:
- Cryotherapy (Ice therapy): Applying ice packs to the affected area helps reduce inflammation and alleviate discomfort.
- Patellar unloading taping: Using specific taping techniques can slightly shift the kneecap to offload pressure from the fat pad, reducing irritation during movement.
- Activity modification: Avoiding deep knee bends, kneeling, and high-impact activities until symptoms improve prevents further aggravation.
2. Restoring Movement and Flexibility
Pain often leads to guarded or restricted movement. Physiotherapists use:
- Manual joint mobilisation: Gentle hands-on techniques help regain full knee extension and flexion, reducing stiffness.
- Soft tissue therapy: Addressing tight muscles like the quadriceps or the patellar tendon to ease tension around the knee.
- Stretching exercises: Focused on the hamstrings, quadriceps, and calves to improve knee mechanics and decrease load on the fat pad.
3. Strengthening for Stability and Tracking
Weakness in muscles controlling the knee can cause patellar maltracking, worsening fat pad impingement. Strengthening is essential:
- Quadriceps strengthening, particularly the vastus medialis oblique (VMO), helps stabilise the patella.
- Hip and gluteal muscle activation improves alignment and reduces inward collapse of the knee during movement.
- Core stability exercises support better posture and efficient movement patterns, indirectly reducing knee stress.
4. Movement Retraining and Prevention
Correcting how you move is just as important as strength:
- Movement pattern correction: Learning proper squat, lunge, and step-down techniques to avoid excessive pressure on the fat pad.
- Gradual return to activities: Slowly increasing the intensity and volume of exercise to build tolerance without flaring symptoms.
- Ergonomic advice: For office workers, adjusting chair height, foot position, and taking regular breaks can reduce knee strain during prolonged sitting.
When Is Surgery Considered?
Most patients respond well to physiotherapy, but if symptoms persist despite conservative care, surgical options may be explored. Arthroscopic procedures can remove inflamed or impinging tissue from the fat pad [7]. However, surgeons aim to preserve as much of the fat pad as possible because of its role in knee nutrition and function [8].
Post-surgical physiotherapy is vital to regain knee motion, strength, and function, preventing stiffness and recurrent pain.
The Bigger Picture: Protecting Your Musculoskeletal Health
Hoffa’s fat pad syndrome is more than a knee problem — it affects your entire musculoskeletal system. Pain can cause you to move differently, placing strain on your hips, back, or other joints. Furthermore, persistent pain may discourage physical activity, leading to muscle weakness and further joint issues.
Early physiotherapy intervention addresses these problems holistically, helping you restore balanced movement, reduce pain, and improve overall function. This proactive approach reduces the risk of future injuries and supports long-term joint health.
Conclusion
Hoffa’s fat pad syndrome is a common yet often overlooked cause of anterior knee pain. Recognising symptoms early and seeking physiotherapy can prevent chronic pain and disability. A carefully tailored rehab programme that controls inflammation, restores motion, strengthens muscles, and retrains movement patterns offers the best chance for full recovery.
Whether you’re a weekend warrior or desk-bound professional, prioritising knee health with expert physiotherapy guidance will keep you moving comfortably for years to come.
https://mysportinjury.janeapp.co.uk/#/staff_member/21/treatment/160 Book a Specialist Physiotherapy Assessment & Examination & treatment (click this link).
References
- Hiba O, Mouha R, Belmoubarik A, Bacheville E, Tawil J. Arthroscopic resection of a chondroma of the Hoffa fat pad: case report and review of literature. Oalib. 2015;2(10):1-4.
- Macchi V, Stocco E, Stecco C, Belluzzi E, Favero M, Porzionato A, et al. The infrapatellar fat pad and the synovial membrane: an anatomo-functional unit. J Anat. 2018;233(2):146-54.
- University football player with Hoffa’s fat pad syndrome: a disablement model case study. Clin Pract Athl Train. 2023;6(2).
- Draghi F, Ferrozzi G, Urciuoli L, Bortolotto C, Bianchi S. Hoffa’s fat pad abnormalities, knee pain and magnetic resonance imaging in daily practice. Insights Imaging. 2016;7(3):373-83.
- Subhawong T, Eng J, Carrino J, Chhabra A. Superolateral Hoffa’s fat pad edema: association with patellofemoral maltracking and impingement. AJR Am J Roentgenol. 2010;195(6):1367-73.
- Jibri Z, Martín D, Mansour R, Kamath S. The association of infrapatellar fat pad oedema with patellar maltracking: a case-control study. Skeletal Radiol. 2011;41(8):925-31.
- Doner G, Noyes F. Arthroscopic resection of fat pad lesions and infrapatellar contractures. Arthrosc Tech. 2014;3(3).
- Nemschak G, Pretterklieber M. The patellar arterial supply via the infrapatellar fat pad (of Hoffa): a combined anatomical and angiographical analysis. Anat Res Int. 2012;2012:1-10.
- Petscavage J, Chew F. Hoffa’s fat-pad inflammation in an HIV-positive patient. Radiol Case Rep. 2010;5(4):446.
- Jarraya M, Diaz L, Roemer F, Arndt W, Goud A, Guermazi A. MRI findings consistent with peripatellar fat pad impingement: how much related to patellofemoral maltracking?. Magn Reson Med Sci. 2018;17(3):195-202.
- Roemer F, Jarraya M, Felson D, Hayashi D, Crema M, Lœuille D, et al. Magnetic resonance imaging of Hoffa’s fat pad and relevance for osteoarthritis research: a narrative review. Osteoarthritis Cartilage. 2016;24(3):383-97.
